|
Quick
Navigation
> General
Information
> Anterior
Instability
> Surgery
for Anterior Instability
> Posterior
Instability
Anterior Instability
Anterior dislocations make up the vast majority
of all instability problems. This occurs when
the ball of the shoulder joint gets forced so
far forwards that the restraints holding the
joint in position tear and the shoulder pops out
of the joint. Often sedation an A&E is
necessary to reduce the shoulder back into its
normal position. Some patients experience
numbness / heaviness in the arm or hand. This is
usually temporary and has occurred because some
of the nerves around the shoulder joint have got
stretched at the time of dislocation.
The natural history
of acute traumatic anterior dislocation of the
shoulder is age dependent.
Age at time of dislocation
Age 13 - 20 Chances of
recurrent instability 80 - 90 %
Age 20 - 30 Chances of recurrent
instability50%
Age 30 + Chances of recurrent instability10%
Age > 40 Chances of recurrent instability
(more likely to have rotator cuff tear)

Treatment
of 1st time dislocation
1. Conservative - External Rotation Bracing /
Sling / Physiotherapy
2. Surgical repair . Arthroscopic / Open
Anterior Stabilisation 2
LINKS
Most shoulder surgeons treat most 1st time
dislocations non-operatively.
There is some limited medical evidence
supporting early surgery in young adults,
usually male, engaged in highly demanding
physical activities with a first time acute
traumatic shoulder dislocation. There is no
strong evidence that early surgical intervention
is beneficial for other categories of patient
(Cochrane Database, Review. August 2006).
Conservative
treatment
After the first time dislocation and reduction
(usually in A&E), the shoulder can be quite
painful. It is necessary to rest and protect the
shoulder in a sling. There is some evidence that
an external rotation brace can reduce the
recurrence rate, but this brace must be applied
within the first 24hrs from dislocation and be
worn continuously, 24hrs per day for 3 to 4
weeks. Any breach in compliance negates all
benefits the brace provided. As compliance with
treatment is so important yet so difficult with
this brace, it is not commonly used. Most
A&E department will immobilize the shoulder
in a standard sling. After the acute pain has
settled it is important to undergo a shoulder
rehabilitation program. This helps settle
discomfort further and may prevent or reduce
future abnormal muscle activations. In doing so,
whilst it does not eliminate recurrence, it may
reduce the frequency of re-dislocation. If
recurrence of shoulder instability occurs after
having had an appropriate rehabilitation program
then the patient must make a choice of either
reconstructive surgery or a lifestyle change to
include activity modification and avoidance of
manoeuvres that put the shoulder joint at risk.
Treatment of
Recurrent Anterior Instability
Usually, I offer my patients surgical
stabilisation of their shoulder joint whenever
they experience their second episode of
instability, having completed my rehabilitative
physiotherapy program or suitable alternative.
Prior to surgery, the anatomy of the shoulder
requires investigation to determine the
magnitude of both soft tissue and bony damage.
These investigations may include simple x-rays,
CT scans and / or MRI / MR arthrogram. The type
of operation performed is determined by both the
structural abnormality and the potential future
demands placed upon the shoulder by the patient.
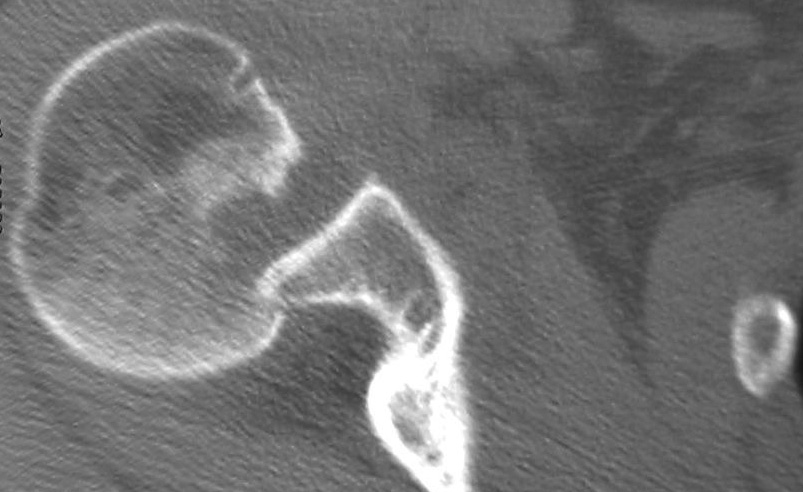 
CT and x-ray showing dislocation of the shoulder
joint
Surgical Options
(a) Soft Tissue:
Bankart Repair
Inferior Capsular Shift
Subscapularis Shortening (Putti-Platt)
Remplissance
(b) Bony Reconstruction:
Bony Bankart Repair
Anterior Bone Block
Laterjet / Bristow
These procedures may be carried out either
arthroscopically (keyhole) or via open surgery.
The results of arthroscopic stabilisation are
comparable to that of open surgery. Arthroscopic
surgery has the advantage over open surgery of
less pain, stiffness, scarring and the ability
to treat other conditions simultaneously. I
reserve open procedures for cases where the soft
tissues are unreconstructable or there is
extensive bone loss from either the glenoid
(socket), or humeral head (ball) sides of the
joint.
The most common
procedure I perform is an Arthroscopic Bankart
repair incorporating an inferior
capsular shift.
Arthroscopic
Anterior Stabilisation (LINK)
Open Anterior Stabilisation (LINK)
|