|
Impingement
Syndrome and Rotator Cuff Disease
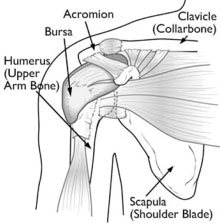
The rotator cuff is an encapsulating sleeve of a
group of tendons that surround the shoulder
joint. These tendons are connected to four
muscles that act to stabilize the shoulder joint
in its socket and to lift and rotate the arm.
The tendons run in spaces (subacromial and
subcoracoid), beneath the shoulder blade,
coracoid process and under the coraco-acromial
ligament where they are vulnerable to injury.
Impingement
Syndrome
Impingement syndrome, is a clinical syndrome
which occurs when the tendons of the rotator
cuff muscles become irritated and inflamed as
they pass through the subacromial space. Pain is
the primary symptom of impingement syndrome and
rotator cuff disease. The pain can be of
gradual, insidious onset, or can be directly
correlated with a single traumatic or an overuse
event (e.g. a day spent trimming hedges). This
pain is poorly localised over the deltoid area
of the shoulder girdle and can occasionally
travel down to the elbow. The pain is increased
when the shoulder is moved away from the side of
the body and patients’have what is called a
“painful arc”. The pain is often worse at night
and aggravated by lying on the affected
shoulder.
Impingement can be caused by extrinsic
mechanical factors , where the space for the
tendon is too narrow, e.g. bony spurs, thickened
ligaments, swollen tendons, or by is intrinsic
factors where the musculo-tendon unit is weak
and unbalanced. Often the cause is a combination
of both.
Impingement is described as occurring in three
stages:
Stage 1:
- reversible oedema and
hemorrhage,
- usually in patients aged 20 – 30 years,
- painful arc of abduction between 60 and 120
degrees.
Stage 2:
- chronic inflammation
leading to fibrosis & thickening of
supraspinatus, biceps, & subacromion
bursa,
- patients are usually between 25-40 years,
- symptoms consist of an aching discomfort,
often interfering with sleep & work, and
may progress to interfere
with activities of daily living.
Stage 3:
- rotator cuff tears,
biceps ruptures, and bone changes,
- significant tendon degeneration,
- patients are usually in the 5th or 6th
decade, and often admit to prolonged
periods of pain, particularly at night;
Other potential causes for
similar shoulder pain are:
- Bursitis
- Calcific tendonitis
- Rotator cuff tear
- Biceps tendinopathy
- AC Joint arthropathy
Treatment
of Impingement Syndrome:
The goal of treatment is to reduce pain and
restore function.
Nonsurgical
Treatment
The vast majority of Stage I and II impingment
syndrome responds well to conservative measures.
Nonsurgical treatment may take several weeks to
months for patients to experience full
resolution of their symptoms.
1. Rest and
activity avoidance
2. Non-steroidal
anti-inflammatory medicines.
3. Physical
therapy. Therapy is initially focused on
restoration of normal range of motion in the
shoulder joint.
Once achieved, the therapist will begin a
program of improving core stability, scapular
stability, cuff strengthening and improved
proprioreceptive feedback.
4. Injection. A
combination of local anaesthetic and steroid is
injected into the subacromial space. This has
the immediate effect of giving temporary pain
relief. The longer term therapeutic effect of
the steroid may take 2 -3 weeks to become
apparent. Rarely, patients can experience a
temporary pro-inflammatory response.

Surgical
Treatment
If non- operative treatment does not provide
long-term relief or if the rotator cuff is at
risk of tear, surgical decompression may be
beneficial.
Arthroscopic
Subacromial Decompression
This is a procedure where bony
spurs and the anterior edge of the undersurface
of the acromion are removed via keyhole surgery.
This operation has a threefold effect of:
1. improving the
physical space available to the tendon,
2. removing any
inflamed bursal tissue,
3. blood products
released from the raw undersurface of the
acromion contain a variety of growth factors and
chemicals that may promote tendon healing.
The Procedure
Most operations are performed as daycase
surgery.
Prior to surgery I recommend that you stop
aspirin or similar medications 7 days prior to
surgery, if it is safe to do so.
I perform the procedure under general
anaesthesia. Before starting surgery I give a
suprascapular nerve block and infiltrate the
subacromial bursa with local anaesthetic. This
is very effective at minimizing post-operative
pain.

The operation itself is
performed through two 5mm incisions, one
posterior and one lateral. An arthroscope ( a
lens about the size and shape of a pencil) with
camera attached is inserted through the
posterior incision. First of all, the
interior of the shoulder joint is inspected for
other pathology, e.g. synovitis, cuff tears,
biceps and labral problems, articular surfaces.
The arthroscope is then inserted into the
subacromial space (above the shoulder joint). A
radiofrequency probe and an electric shaver are
inserted through the lateral portal (incision).
The bursa is excised, the coraco-acromial
ligament is often resected. The bony spur and
4mm of bone are resected from the anterior
acromion , the acromioclavicular joint is not
violated.
Any other pathology found at
time of surgery is also treated. Skin sutures
are not necessary. Simple adhesive plasters
cover the wound.
Post-operative
Care
Immediately following your surgery:
- you will have an absorbent dressing covering
you shoulder for 24 hours to absorb the
arthroscopic fluid that was pumped through your
shoulder during the procedure.
- you will have an icepack to help reduce post
op inflammation. I recommend it is applied for
30 -45 minutes and then removed for 2 hours
before being re-applied. This has been shown to
be effective for up to 72 hours post surgery.
- your arm will be supported in a sling. This is
for comfort and pain relief. It is possible that
you will need to wear this for 1 – 2 weeks.
- Physiotherapy can commence when the
post-operative pain begins to settle. It is
important to be guided by your therapist and not
to overdo your exercises.
Post-operative
physiotherapy program
Following discharge from hospital you will have
regular outpatient review until your symptoms
are significantly resolved.
Outcome
The pain of impingement syndrome mostly comes
from the rotator cuff tendon. Arthroscopic
SubAcromial Decompression is effective at
improving symptoms in about 85% of cases .
Whilst the operation increases the mechanical
space available for the rotator cuff, it also
functions to promote your body’s own healing
response. This response can take 9 – 12 months
to attain maximum benefit. A general rule of
thumb is that you can expect to get better at a
rate of 10% reduction in pain levels per month.
Complications of
surgery
Complications following arthroscopic subacromial
decompression are rare but can include:
Post operative stiffness – usually temporary
Infection
Nerve irritability
ACJ pain – occasionally pre-existing but
asymptomatic problems with the AC joint can be
unmasked once subacromial symptoms are
alleviated.
|